
Increasingly, researchers are concluding that the diets of people with mental health disorders are lacking in key nutrients for brain health. And they’re finding that replenishing these nutrients can play an important role in treating those disorders. “Nutritional psychiatry” is a fast-growing approach that uses food and supplements in the treatment of mental health conditions.
The Science Behind Nutritional Psychiatry
A growing body of scientific evidence suggests that nutritional treatment may help prevent, treat, or improve depression, bipolar disorder, schizophrenia, anxiety, ADD/ADHD, autism, addiction, and eating disorders. And the scientific community is finally beginning to see how food is so strongly linked to brain health/mental health.
In 2015, a group of 18 scientists concluded that “the emerging and compelling evidence for nutrition as a crucial factor in the high prevalence and incidence of mental disorders suggests that diet is as important to psychiatry as it is to cardiology, endocrinology, and gastroenterology.”
“…diet is as important to psychiatry as it is to cardiology, endocrinology, and gastroenterology.” —The Lancet Psychiatry
In 2017, a 12-week study known as the “SMILES trial” looked at the impact of dietary support compared with social support in 67 people with moderate to severe depression who ate unhealthy diets. After the 12-week trial, 32% of those receiving dietary support achieved remission compared with only 8% of those in the social support group.
As the evidence mounts, it’s clear that what you put in your mouth matters when it comes to mental health/brain health. But when it comes to diet and nutrition, there are so many mixed messages about what’s healthy and what isn’t. What should you eat?
Making Food Insanely Simple
Yes, there is a lot of conflicting health information about food, but there is also a lot of agreement. If you follow these 11 rules your mental health/brain health will start to improve within days.
Only love foods that love you back.
So, you love Hot Cheetos, but do they love you back? They’re filled with pro-inflammatory vegetable oils, sugar that promotes brain aging, and MSG and red dye #40, which can worsen ADD/ADHD symptoms and can cause “mind-storms.”
Go for the highest quality calories you can find, and not too many of them if you need to lose weight.
Calories matter! If you supersize your meals, you’ll supersize your body. And obesity is associated with a smaller brain and increased risk for depression and Alzheimer’s disease.
Hydrate, but do not drink your calories.
Your brain is comprised of 80% water and being even mildly dehydrated can negatively impact your moods—making you feel more anxious, tense, depressed, or angry—in addition to sapping your energy levels and lowering your ability to concentrate. Skip the high-calorie coffee concoctions, sodas, and fruit juices.
Eat high-quality protein at every meal.
It balances blood sugar for more stable moods and keeps cravings away.
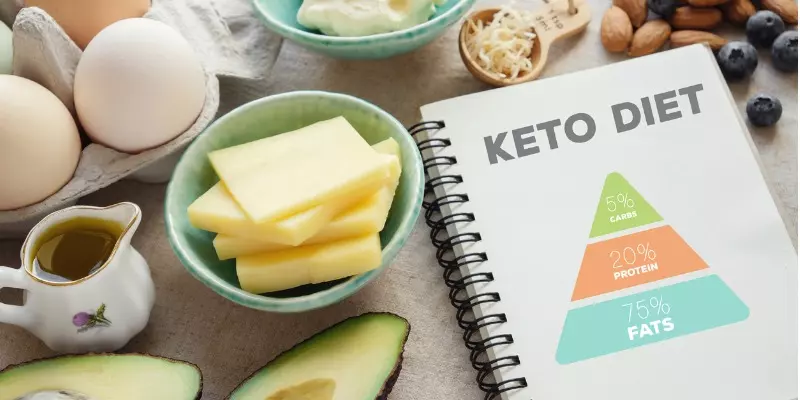
Eat and cook with high-quality fat
Did you know that 60% of the solid weight of your brain is fat? Low-fat diets are not good for your brain. Focus on healthy fats, such as avocados, nuts, seeds, and sustainable, clean fish. Fat is not the enemy. Good fats are essential to your mental health/brain health. For example, omega-3 fatty acids have been found to reduce symptoms of depression.
Go for smart carbohydrates (colorful, low glycemic, and high fiber).
Colorful fruits and vegetables boost the level of antioxidants in your body, which reduces the risk of developing cognitive impairment and depression.
Use herbs and spices like medicine.
For example, in multiple studies, a saffron extract was found to be as effective as antidepressant medication in treating people with major depression
Make your food as clean as possible.
Eliminate artificial sweeteners, colors, preservatives, and foods in plastic containers.—Read the labels.
If you struggle with any brain health/mental health or physical issue, eliminate any potential allergens or internal attackers.
Such as sugar, MSG, gluten, corn, soy, and dairy for a month to see if your symptoms improve.
Use intermittent fasting to supercharge your brain.
Intermittent fasting, or “time-restricted feeding,” has been shown to significantly improve memory and mood.
Get a routine that serves your health rather than hurts it.
Find 25 foods you love that love you back.
If you or a loved one are struggling with anxiety, depression, trouble concentrating, brain fog, or other signs of mental health disorders, understand that finding the root cause of those symptoms is key to getting well. At Amen Clinics, we use brain SPECT imaging to detect brain patterns associated with various disorders and to help us develop a personalized treatment. For over 30 years at Amen Clinics, we have been helping thousands of people by using the least toxic, most effective solutions, including nutrition coaching, supplements, helpful forms of psychotherapy, and much more.
Speak to a specialist today at 888-288-9834 or schedule a visit online.



What’s derealization? Can it be treated? I think that would be a great podcast subject.
Comment by Mandy Andrei — February 14, 2020 @ 4:34 AM
Great article! The only part I might have to argue with is the suggestion of intermittent fasting. My daughter was in treatment for an eating disorder a few years ago and I have become educated as to the plethora of societal messages that this illness twists in the minds of it’s victims. The number of people currently battling an eating disorder combined with the number of people who are in remission is a severly under reported number. There are not enough treatment facilities. Insurance tries to shorten treatment time and cut costs. It just seems to me that there are so very many uphill battles and when January / February rolls around and all that you see are ads for weight loss and limited or eliminating food – the message can severely deter recovery.
Sandra Burt
Comment by Sandra Burt — February 14, 2020 @ 5:09 AM
I am 85 years old. Most of the time I am dizzie or foggie. I take Meclizine for Vertigo, even tho I never been tested.
What should I do?
Comment by Shirley Sellers — February 14, 2020 @ 5:17 AM
I, just recently added your newsletter. I, know your findings are correct. I, couldn’t begin to give the list of labels, that probably fit me. I’ve never had a diagnosis. But I’ve suffered with everything from uncontrollable rage and outbursts among other emotional problems. I, have symptoms of add, or is it adhd? Bi polar mood swings and all kinds of other hard things to deal with. I will have a year sober tomorrow. I have been off sugar for less and I quit processed and unhealthy carbohydrates in November. After a month long withdrawal from carbs, %90 of my symptoms just vanished. I haven’t had a mood swing since November 17th… my wife and family can’t understand., we’re amazed. We had all given up. I thought I needed a mental hospital while withdrawing the carbs. And like I said, then it passed. I take my diet so seriously now. My wife and I have a 5 year old non verbal child at home (Leiah), I sure wish getting her off the carbs and stuff would be as easy. Twice as hard with a child and ten times harder with a non verbal anyone… I wish we were doing better financially. The lot of us would come out for brain scans. The findings and help they could offer may not even be quantifiable. My bank account and charge cards can be though… not sure why I’m sending this. Yes I’d love help and insight. I realize nothing is free. So for now I just read and learn what I can.
Thank you, for taking the time to read this, and have a great day,
Joe David
Comment by Joseph David — February 14, 2020 @ 6:56 AM
I think that people recommend IF for the benefit of autophagy. As well, once fat-adapted, for someone like me with a super slow metabolism it has proven to be quite useful in reversing both fatty liver and abdominal fat. I agree with you that for someone with an eating disorder it is probably a bad idea. Those of us with metabolic syndrome can surely benefit from smaller feeding windows. As well, the combination of low-carb carnivorish and IF has been a God send for my adult ADHD mind! Brain fog is gone!
Comment by Jennifer Crosby — February 14, 2020 @ 3:39 PM
Congratulations Joseph! So glad you are sober and feeling better on a clean diet. Best of luck with your daughter.
Comment by Connie — February 14, 2020 @ 5:16 PM
There is a lot of evidece that intermittent fasting is beneficial for the brain. Perhaps its not as good for those with eating disorders, but in general, there are benefits for the general population.
Comment by David — February 14, 2020 @ 8:45 PM
I read your comments and am grateful you found helpful information to bring about such positive change. Amazing. I was moved to stop and pray for you and your wife and daughter.
Comment by Tina Marie — February 15, 2020 @ 1:58 AM
I’m not a doctor so this is just an idea. My transition off carbs (this time) has lasted because I added some good fats to my diet. I was binge eating any carb I could reach. Now there is no problem and I am slowly losing weight and have the energy to do mild exercises. Brain fog is pretty much gone and I don’t need to sleep 18 hours a day. Adderall and Ritalin made no impact. I have ADHD. Good luck on your non-verbal little one. I hear you
on budget issues.
Comment by ELAINE SMITH — February 15, 2020 @ 8:05 AM
What is your recommend for studying nutritional psychiatry? There are no degree programs out there that I am aware of.
Please advise and thank you
Comment by Jennie — February 15, 2020 @ 10:47 PM
Can you explain what intermittent fasting is?
Comment by karen van couvering — February 17, 2020 @ 4:34 PM
Have you studied HCVs effect on the CNS? I’m post tx 5 years.
Comment by Janice Mitchell — February 19, 2020 @ 1:37 PM
Joe, Thank you for sharing your story and congratulations. It may help a lot of people. It is hard to talk about some things, but I think you have done a great job here. And, like you, I think many of us would go for the brain scans but we can’t afford it. Good luck with your daughter.
Diana
Comment by Diana Maykowskyj — February 20, 2020 @ 2:24 PM
Re: derealization. For a clinical description, look to the medical establishment. But Just a brief observation of my own: I’ve experienced Benzodiazapine Withdrawal Syndrome while stopping clonazepam (Klonopin) cold-turkey. (NEVER attempt this; seizures can occur, and the consequences can be fatal in some cases!) The BWS was something I learned about on my own- it was severe, but I suffered in silence. When I learned about BWS I realized it was what I had experienced. Both the physical and psychological symptoms were unmistakable in retrospect, and it was no coincidence that they occurred just days after my last dose of medicine (I had developed a physical dependence, though I wouldn’t necessarily say ‘addiction’. A clinician may disagree). Anyway, one side effect of withdrawal was a sense of derealization or depersonalization. There seemed a ‘screen’ or veil between myself and the environment, and the anxiety naturally made me feel detached from myself. Everything seemed…surreal. It’s one of the hallmarks of BWS. In many cases, anxiety causes a feeling of separation from self, others and the environment. It is difficult to describe precisely, but ‘you know it when you feel it’. I’ve also had episodes of acute derealization during and after panic attacks, and milder bouts amid generalized/free-floating anxiety. Thankfully it has been many years since I’ve experienced this unnerving sensation. If you think you may be experiencing similar feelings, whatever the cause may be (they can vary widely), do some further reading and think about consulting a doctor. All the best.
Comment by peter walsh — April 19, 2020 @ 7:41 AM