Dual Diagnosis
Unlike traditional psychiatry, which rarely looks at the brain, Amen Clinics uses brain imaging technology to identify brain patterns associated with both addictions and mental health conditions.
What is Dual Diagnosis?
Dual diagnosis (also referred to as co-occurring conditions or comorbidities) is a term used for people who are struggling with both a mental health condition and a substance use disorder. In some people, these multiple disorders develop at the same time, while in others, either one of the conditions can precede the other. In the traditional healthcare system, it can be very hard to get an accurate diagnosis of both addiction and mental illness. Symptoms of substance abuse or withdrawal can be similar to those of certain mental health conditions, so it’s possible for providers to miss an underlying psychiatric disorder. Getting an accurate dual diagnosis is critical to healing and recovery. Addressing the underlying mental health condition and brain-related issues is the key to helping you be successful in an addiction treatment program.
Who has Dual Diagnosis?
Approximately 7.9 million American adults have both a mental health condition and substance use disorder, according to a 2014 National Survey on Drug Use and Health. Among adolescents aged 12-17, the percentage who use drugs is higher in those who have depression. Young people in this age group with depression are more likely to use marijuana, hallucinogens, inhalants, and prescription drugs and to be heavy drinkers. Among adolescents seeking treatment for substance abuse, 50-90% also suffer from some form of psychiatric disorder.
What are the Symptoms?
Considering there are so many different mental health conditions that can co-occur with addiction, there can be a wide range of symptoms with dual diagnosis. Symptoms of substance use disorders may include:
- Neglecting responsibilities
- Stealing to fuel your addiction
- Withdrawal from family and friends
- Feeling powerless to change your habit
- Feelings of guilt about your substance use
- Using increasing amounts of the substance
- Inability to quit without withdrawal symptoms
- Getting defensive when someone questions your habits
- Feeling like you need the substance in order to function
- Impulsivity, nervousness, feeling numb and more.
What Causes Dual Diagnosis?
A number of factors may contribute to dual diagnosis, including brain abnormalities, genetics, head injuries, or exposure to stress or environmental toxins. (See below for more information on the causes of dual diagnosis.)

Symptoms of co-occurring mental health conditions can include:
- Impulsivity
- Nervousness
- Hopelessness
- Feeling numb
- Extreme mood swings
- Trouble concentrating
- Confusion
- Suicidal thoughts
Why Choose Amen Clinics for Treating Dual Diagnosis?
At Amen Clinics, we use brain SPECT imaging as part of a comprehensive evaluation to diagnose and treat people struggling with addictions and mental health disorders. Based on our brain imaging work, we have identified 6 types of brain patterns associated with addiction and 7 types of depression, anxiety, and ADD/ADHD. Knowing your type is key to getting the most effective treatment. In addition, we assess any biological, psychological, social, and spiritual factors that may be contributing to dual diagnosis.
Dual Diagnosis Brains Work Differently
Having both addiction and a mental health disorder means there are multiple issues in the brain. On the addiction side, it’s a problem with the brain’s reward system—an intricate network of brain circuits and neurotransmitters that work together to drive you to seek out rewarding things (such as food and sex) but that regulate self-control so you don’t overdo it. In people with addictions, however, the brain’s drive circuits (the nucleus accumbens and deep limbic system) dominate, and the self-control circuit (the prefrontal cortex) doesn’t work hard enough. The result is a lack of self-restraint and for some people, addiction to substances like drugs and alcohol. Even if you suffer consequences from drinking too much or taking drugs, the dysfunction in your brain’s reward system pushes you to repeat the behavior over and over again. On the mental health side, a variety of brain regions may be involved depending on the condition or conditions.
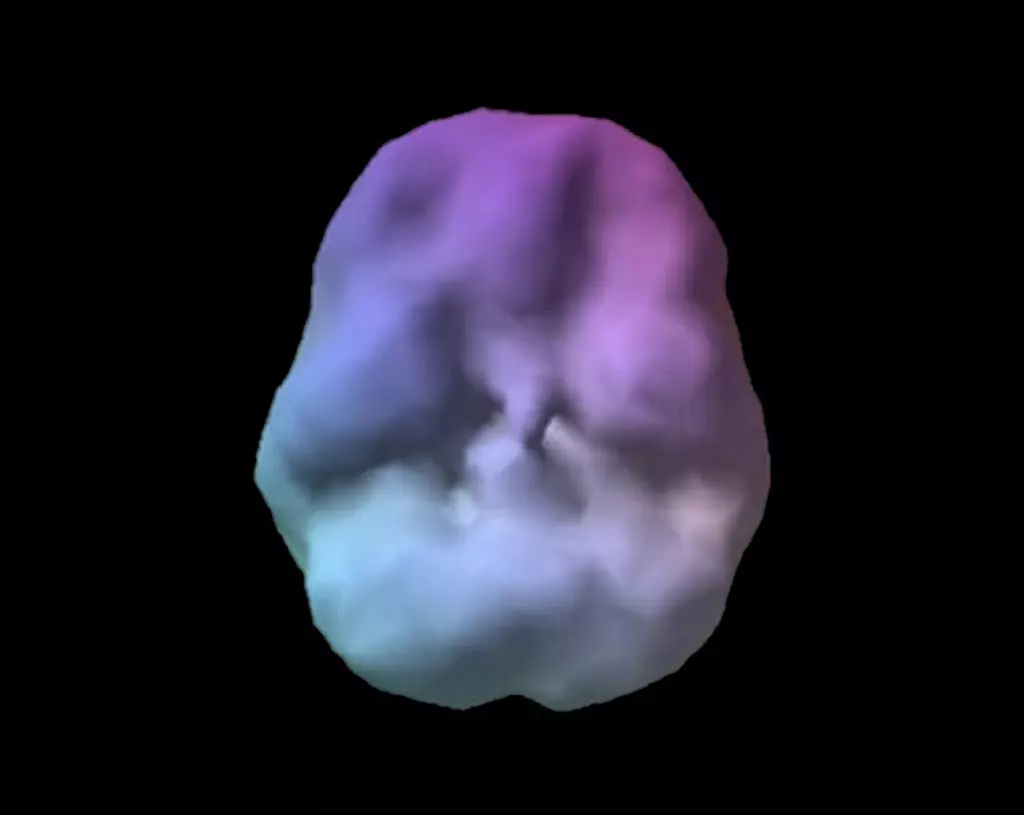
Healthy Brain Scan

Dual Diagnosis Brain Scan
SPECT (single photon emission computed tomography) is a nuclear medicine study that evaluates blood flow and activity in the brain. Basically, it shows three things: healthy activity, too little activity, or too much activity. The healthy surface brain SPECT scan on the left shows full, even symmetrical activity. The SPECT brain images of substance abusers (like the one on the right above) typically have an overall toxic appearance. They look less active, more shriveled, and have a scalloping effect. The holes do not represent actual physical holes in the brain, they represent areas that are low in blood flow and activity.
Ready to learn more? Speak to a care coordinator today!
Contact UsWhat Causes Dual Diagnosis?
A number of factors may contribute to addiction and mental illness.
- Brain abnormalities: Based on the world’s largest database of brain scans related to behavior—over 200,000 and growing—it has become clear that mental health conditions and addiction issues are actually brain problems.
- Genetics: Some genes may predispose certain people to a vulnerability for addiction and mental health problems.
- Exposure to trauma or stress: People who have experienced trauma are at a much higher risk of developing a mental health condition and are also at increased risk of substance use disorders.
- Head Injuries: Brain imaging studies show that even mild physical trauma can damage the brain and increase your risk of addiction and mental health problems. Alcoholism and drug abuse, as well as ADD/ADHD, anxiety, and depression are all more common in people who have experienced head injuries.
- Exposure to environmental toxins: Common environmental toxins, such as mold, insecticides, tobacco smoke, paint, nail polish, and phthalates (found in thousands of plastic products), pose a risk to brain function and increase the incidence of brain disorders, such as ADD/ADHD. Brain scans of indoor painters show some of the highest levels of brain damage. Any damage to the brain can increase your vulnerability to addiction.
- Dementia: Dementia has been linked to an increased risk of addiction and compulsive behaviors. When elderly people who have lived their entire lives without a problem suddenly start abusing drugs or alcohol and suffering from a mental health condition, it’s worth investigating if some form of dementia may be involved.
“Knowing About Your Brain Can Help Yourself and Others”
– Daniel G. Amen, M.D.
Common Co-Occurring Conditions
Addictions may occur with any mental health disorder, but some of the more common conditions include:
- ADD/ADHD: Children and adults with untreated ADD/ADHD are also at increased risk for addiction. According to one study, half of all people with ADHD will develop a substance abuse problem if it remains untreated. A 2005 report in the journal Pediatrics found that having prior or current ADHD also makes you more prone to become addicted at an earlier age and results in a greater intensity of abuse.
- Anxiety: People with anxiety are twice as likely to abuse drugs and alcohol compared with the general population, according to the National Institute on Drug Abuse.https://www.amenclinics.com/conditions/depression/
- Depression: Substance abuse is about twice as common in depressed people as in people who don’t have this condition. Many people with depression use alcohol to numb their feelings, but alcohol is a central nervous system depressant that can trigger symptoms associated with depression.
- Post-Traumatic Stress Disorder (PTSD): Some studies suggest that over half of all people with PTSD also struggle with substance abuse.
- Bipolar Disorder: People with bipolar disorder may use drugs and alcohol as a coping mechanism for their mood swings, but research also shows that drug abuse may cause changes in the brain that contribute to the development of bipolar disorder.
- Schizophrenia: About half of all people suffering from schizophrenia report having abused drugs and/or alcohol. Many drugs, including marijuana, can increase the severity of schizophrenia symptoms.
- Psychosis: There is an increased risk of psychosis in people who use marijuana.
