Obsessive Compulsive Spectrum Disorders
Unlike traditional psychiatry, which rarely looks at the brain, Amen Clinics uses brain imaging technology to identify brain patterns associated with obsessive compulsive disorder and related conditions.
What is Obsessive-Compulsive Disorder?
Obsessive-compulsive disorder (OCD) is a serious and often debilitating mental health condition that is characterized by obsessions—intrusive thoughts, images, or urges—and/or repetitive behaviors, called compulsions, that help to neutralize the distress caused by the obsessions. While most people have distasteful and unpleasant thoughts from time to time, they tend to pass pretty quickly and do not get stuck in an endless loop inside their head. However, this is not the case for people who suffer with OCD. Left untreated, their persistent obsessions and compulsive rituals can take over their life and lead to significant problems with personal, interpersonal, occupational, academic, and social functioning.
Who Has OCD?
In the U.S., the prevalence of OCD in the population is about 1.2%. The average age of onset is between 19 and 20, and it is somewhat unusual—but not impossible—for OCD to begin after a person is in their mid-30s. This condition affects males and females equally, but boys tend to be diagnosed at a younger age than girls. It is estimated that 25% of boys with OCD develop symptoms prior to age 10.
What are Common Symptoms of OCD?
Obsessions are unwanted recurring thoughts, impulses, or mental images that are usually senseless, sometimes frightening, and often repulsive. These thoughts can trigger distressing feelings of anxiety or disgust. People with OCD often make a great effort to suppress or resist their obsessions, but the more a person tries to control them, the more powerful they can become.
Obsessions often involve repetitive thoughts and fears about:
- Germs or contamination
- Forbidden sexuality
- Harm or violence
- Losing control
- Religion
- A need for symmetry or perfectionism

Untreated OCD can have alarming consequences and is associated with higher incidences of:
- Decreased concentration
- Short-term memory problems
- Job failure
- Academic failure
- Social isolation
- Physical exhaustion
- Emotional exhaustion
- Substance abuse
- Depression
- Panic attacks
- Suicidal thoughts
Compulsions are behaviors that are performed persistently and repetitively, even though they do not lead to an actual reward or pleasure. They are usually an attempt to make the obsessions subside and to reduce the anxiety caused by them. Inside, a person with compulsions experiences an urgent insistent sense of “I have to do it” and performs the compulsive behavior according to certain rules in a very strict or rigid manner and can result in elaborate, time-consuming rituals.
The most common compulsions include:
- Excessive washing, especially the hands
- Extreme and needless cleaning, such as in the household
- Counting, including wanting to end on a “good” or “safe” number
- Repeating things, such as certain names, phrases, or prayers
- Checking a specific number of times, such as repetitively checking the door is locked or the stove is turned off
- Touching things, often in a particular sequence
- Arranging objects in a precise or symmetrical way
Many people with OCD recognize that their obsessive thoughts are senseless and that their compulsions are outside the realm of normal behavior, yet they can’t control them. Other individuals with the condition don’t see that there’s anything abnormal about their thoughts or behaviors. For example, with children, it is more likely to be a parent or teacher who notices the distressing symptoms.
What Causes OCD?
Although the exact cause of OCD is not fully understood, studies have shown that a combination of biological and environmental factors may be involved. Research has found that OCD tends to run in families. Having a first-degree relative with it doubles the risk for it. However, if a first-degree relative developed the disorder in childhood, the risk jumps to 10 times that of someone without a familial history of OCD. Environmental factors such as childhood abuse or other trauma and stressors can increase the risk for obsessive-compulsive disorder. Infections, like Lyme disease and PANDAS (pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections), can elevate the chances of developing OCD symptoms. Research has also found that up to 25% of people with epilepsy have OCD too.
The course of OCD is quite varied. Symptoms may come and go, ease over time, or get worse. If the symptoms become severe, this condition can prevent a person from working or carrying out normal responsibilities at home.
Why Choose Amen Clinics for Treating OCD?
At Amen Clinics, we take a unique brain-body approach to evaluation that includes brain SPECT imaging to make an accurate diagnosis of OCD. This helps our doctors understand the underlying cause of each patient’s obsessive-compulsive symptoms so that a targeted and personalized treatment plan can be created.
OCD Brains Work Differently
In people with OCSD, brain SPECT studies have shown increased blood flow specifically in two regions of the brain—the basal ganglia and anterior cingulate gyrus.
- Basal ganglia: This region helps set the body’s anxiety level and is involved in forming habits. When there is too much activity in the basal ganglia, it is associated with increased anxiety and heightened fear.
- Anterior cingulate gyrus (ACG): This area is involved in helping people to shift their attention from subject to subject. When the ACG is overactive, people tend to get “stuck” on the same thoughts or behaviors.
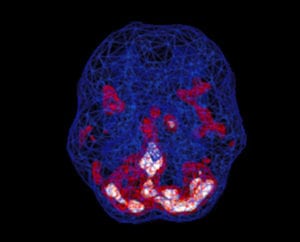
Healthy Brain Scan

OCD Brain Scan
SPECT (single photon emission computed tomography) is a nuclear medicine study that evaluates activity (blood flow) in the brain. Basically, it shows three things: healthy activity, too little activity, or too much activity. In a healthy “active” scan, blue represents average blood flow and red and white represent increasingly higher levels of blood flow. In the healthy scan on the left, the most active area is the cerebellum, at the back/bottom part of the brain, which is normal. In the OCD brain on the right, there is overactivity in several areas of the brain including the anterior cingulate gyrus and basal ganglia.
Ready to learn more? Speak to a care coordinator today!
Contact UsRelated Conditions with Obsessive and/or Compulsive Behaviors
In addition to OCD, there are other conditions that have obsessive-compulsive qualities, including:
- Trichotillomania (repeatedly pulling out hair from the body, most often from the head, eyebrows, and eyelashes)
- Excoriation (skin picking to the point that it causes sores on the body)
- Hoarding disorder (abnormal fear of discarding possessions and other items, even trash)
- Body dysmorphic disorder (an unremitting preoccupation with perceived physical flaws that aren’t really noticeable to others)
- Onychophagia (frequent and sometimes uncontrollable biting or chewing on fingernails)
Why Misdiagnosis and Improper Treatment is Common
Many mental health conditions can be misdiagnosed, but OCD is one of the more likely ones to be mistaken for other conditions because it has so many overlapping symptoms. In fact, a 2015 study among primary care physicians found that half of OCD cases were incorrectly diagnosed. OCD can be misdiagnosed as ADD/ADHD, anxiety, bipolar disorder, autism spectrum disorder, PTSD, or schizophrenia.
Getting an accurate diagnosis is critical since the treatments for these conditions differ dramatically. And the wrong treatment plan can make a person with OCD worse. For example, giving stimulant medication, which is commonly used to treat ADD/ADHD, can exacerbate some OCD symptoms.
In addition, like many other conditions, OCD is not just a single and simple disorder. In terms of treatment, one size does NOT fit all. Giving everyone who has OCD the same treatment may help some people but can make others worse. It is imperative to find out what is causing the obsessive-compulsive symptoms a patient is experiencing and treat the underlying cause, rather than taking a cookie-cutter approach that only masks the symptoms.
“With A Better Brain Comes A Better Life”
– Daniel G. Amen, M.D.