Schizophrenia and Schizoaffective Disorders
Unlike traditional psychiatry, which rarely looks at the brain, Amen Clinics uses brain imaging technology to help identify underlying brain issues associated with psychosis and schizophrenia spectrum disorders.
What are Schizophrenia and Schizoaffective Disorders?
Psychosis and schizophrenia spectrum disorders are very complex, and at times, disabling mental health issues that are tightly connected. In the section below, we will describe the differences and links between them.
Psychosis
The term psychosis is characterized by an inability to distinguish reality from what is not real. This may happen briefly, episodically, or for extended periods of time. Losing touch with the “real world” in this way is referred to as a psychotic episode and may lead to a diagnosis of some type of psychotic disorder. It is estimated that 3% of people will experience psychosis during their lifetime.
Psychosis is not a mental health condition per se, but rather a syndrome that generally refers to two main types of symptoms:
Delusions
These are false beliefs a person holds tightly to despite a complete lack of evidence for them. Delusions tend to fall into certain themes that center around persecution, jealousy, grandiosity, body sensations and functions, and believing an unknown person loves them.
Hallucinations
When people have auditory hallucinations, they hear things outside of their head, such as a voice telling them to do something, even though there is no one actually speaking. Similarly, during visual hallucination, someone will see things outside of themselves that no one else can see. And during tactile hallucinations, an individual will experience abnormal sensations inside or on their body (i.e. bugs crawling on their organs).
Regardless of the type of hallucination or delusion a person is having, it feels completely real to them.

Consequences of untreated psychosis and schizophrenia spectrum disorders include:
- Homelessness
- Relationship conflicts
- Poverty
- Joblessness
- Inability to complete schooling
- Substance abuse
- Anxiety and Phobias
- Depression
- Social isolation
- Self-harm and Suicidality
What Causes Psychosis?
Psychosis can be caused by many different things; however, it is most common in certain mental health condition, including:
- bipolar disorder
- major depression
- postpartum depression
- schizophrenia spectrum and other psychotic disorders, which are described in greater detail below
Psychosis can also be caused by an infection that impacts the brain, head trauma, hormonal imbalances, insomnia, some medications, alcohol and substance abuse, medical illnesses, and neurological disorders.
Schizophrenia Spectrum Disorders
Schizophrenia spectrum disorders fall into a category of mental health conditions known as psychotic disorders. The severity, symptomology, and duration of these conditions vary; however, they share many of the same characteristics that are typically grouped into three categories:
1. Positive Symptoms: Hallucinations (hearing voices, seeing people, animals, objects, or other things, or feeling tactile sensations that aren’t there), delusions, agitated or abnormal body movements, and disorganized speech, thinking, and behavior
2. Negative Symptoms: Decreased sense of pleasure in life, trouble initiating and following through with activities—even self-care, difficulty maintaining relationships, social withdrawal, speaking less, and emotional flatness
3. Cognitive Symptoms: Decreased executive function (processing incoming information, decision-making, etc.), difficulty with concentration and focus, trouble with memory, and lack of awareness that they have a mental health disorder.
Why Choose Amen Clinics for Treating Schizophrenia and Schizoaffective Disorder?
Psychosis and schizophrenia spectrum disorders are often misdiagnosed for a variety of reasons. This is why we use brain SPECT imaging at Amen Clinics as part of a comprehensive evaluation to diagnose and treat our patients. We also assess other factors—biological, psychological, social, and spiritual—that can contribute to psychotic disorders. Based on all this information, we are able to personalize treatment using the least toxic, most effective solutions for a better outcome for each patient.
Psychotic and Schizophrenia Spectrum Brains Work Differently
These disorders are complex and involve several brain areas. Abnormalities in the neurotransmitters dopamine and glutamate—and possibly others—cause decreased activity in the prefrontal cortex (the area of the brain involved in decision-making, judgment, forethought, attention, impulse control, and more). Brain SPECT imaging studies on people with schizophrenia and psychotic disorders can reveal brain abnormalities that interfere with information processing.
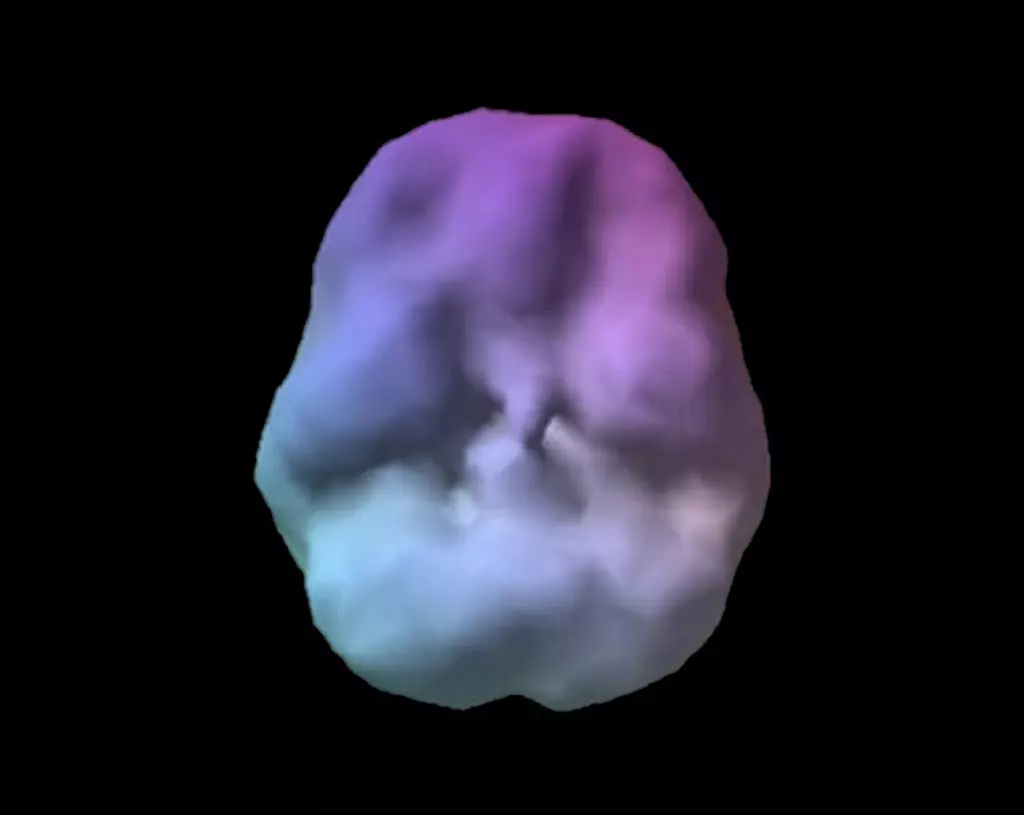
Healthy Brain Scan

Schizophrenic Brain Scan
SPECT (single photon emission computed tomography) is a nuclear medicine study that evaluates activity (blood flow) in the brain. Basically, it shows 3 things: healthy activity, too little activity, or too much activity. The healthy surface brain SPECT scan on the left shows full, even symmetrical activity. The brain scan on the right of a patient named Steve with schizophrenia (read more about Steve below) shows high levels of damage and overall decreased activity.
Ready to learn more? Speak to a care coordinator today!
Contact UsTypes of Schizophrenia Spectrum and Other Psychotic Disorders
In addition to the schizophrenia spectrum disorders, there are other psychotic disorders. While each condition in this category reflects some degree of psychosis, there is a varied presentation of psychopathology within them. The following section gives an overview of each one to provide a general understanding of these very serious mental health conditions.
Schizophrenia
A severe and debilitating psychotic disorder, schizophrenia is often a chronic condition that affects about 1% of the U.S. population. It is characterized by delusions, hallucinations, and disorganized speech, thinking, and behavior as well as negative symptoms, such as emotional flatness and lack of initiation. Symptoms typically emerge in males during late adolescence to early 20s and in females in the late 20s to early 30s, although there is some variability with age onset.
There is thought to be a genetic component in schizophrenia. Research has found possible abnormalities in neurotransmitter activity in this disorder, although the exact mechanisms are still being studied. Additional risk factors include childhood adversity, oppression and discrimination, poverty, and other psychosocial factors.
People with schizophrenia have an increased risk for co-occurring conditions, such as anxiety, obsessive-compulsive disorder, and tobacco use disorder. Sadly, 20% of individuals with schizophrenia will attempt suicide at least once, and 5%-6% will take their own life.
Schizophreniform Disorder
The symptoms of this condition are largely the same as in schizophrenia. What sets them apart is that in schizophreniform disorder, an episode of symptoms will last between 1 and 6 months, whereas in schizophrenia symptoms last at least 6 months and often much longer. It is estimated that approximately 33% of people who are diagnosed with schizophreniform disorder won’t progress to a more severe condition. However, the other two-thirds will eventually be diagnosed with schizophrenia or schizoaffective disorder.
Schizoaffective Disorder
In schizoaffective disorder, a person will have an episode of either mania or major depression at the same time they have positive and negative symptoms of schizophrenia (described above). Once the mood episode has passed, the psychotic symptoms persist for at least 2 weeks afterward. As in schizophrenia, 5% of people with this very challenging disorder will die by suicide. Although it typically develops in early adulthood, schizoaffective disorder can emerge any time from adolescence on—even later in life.
Schizotypal Personality Disorder
People with schizotypal personality disorder display eccentric behaviors and have an uneasiness with interpersonal functioning as well as deficits in interacting with others. They are socially anxious and often have paranoid, strange, superstitious, or unusual beliefs. Stress may trigger psychotic episodes in those who have schizotypal personality disorder. It is estimated that slightly over 3% of the U.S. population have this condition, which does not change much during a person’s lifetime. However, a small percentage of people who have it will develop schizophrenia or a related psychotic disorder.
Delusional Disorder
As the name of this condition implies, people with it have delusions—false beliefs to which they hold tightly despite an absence of evidence that they are true or real. Delusions frequently fall into specific themes, such as these:
- Persecutory delusions—the belief that someone or a group of others intends to cause some kind of harm to the person. This is the most common type of delusion.
- Grandiose delusions—falsely believing they have extraordinary abilities (albeit unrecognized), notoriety, or financial success
- Erotomanic delusions—erroneous belief that someone, usually a person they don’t know (i.e. a famous actor) is in love with them
- Jealous delusions—believing that one’s spouse or significant other is being unfaithful, even though they are not. This delusion is more common in men than women.
- Somatic delusions—these involve imagined sensations and/or functions in the body
Although there is generally less impairment in this condition compared to other psychotic disorders, problems in social, relational, and occupational functioning as a result of their false, delusional beliefs are common. There is a genetic link between delusional disorder and both schizophrenia and schizotypal personality disorder. And some individuals with delusional disorder will eventually develop schizophrenia.
Brief Psychotic Disorder
What separates brief psychotic disorder from other psychotic conditions is that there is a quick onset of symptoms which includes at least one of these: delusions, hallucinations, or incoherent/bizarre speech. The symptoms last anywhere from a single day to a full month. Even though this mental illness is a shorter course than the other psychotic disorders, the symptoms are very intense and distressing and can cause significant impairment in functioning as well as an increased risk for suicide. Often, patients will need to be hospitalized until they become stable, but once the episode has fully resolved, they return to their normal level of functioning. Brief psychotic disorder can emerge at almost any time during a person’s lifespan, and half of the people who have one episode will have another at some point. Although there is not a single cause for this condition, it has been known to occur during postpartum or very stressful periods.
Substance- or Medication-Induced Psychotic Disorder
Not surprisingly, substance and alcohol abuse can lead to a psychotic episode. In some cases, it might come from excessive intake, such as a period of very heavy drinking or a cocaine binge. In other cases, psychosis can occur during withdrawal from drugs or alcohol. In one study, 74% of people with first episode psychosis had a substance use disorder at some point during their life. Cannabis, LSD, alcohol, amphetamines, cocaine, and other substances are associated with an increased risk of psychosis in people who have an underlying predisposition.
It is also possible to become psychotic from prescribed pharmaceutical medications (that are not being abused), including some common antibiotics, muscle relaxants, pain relievers, Parkinsonian medications, and others. Some people, especially older individuals who are taking several medications for medical issues can develop psychosis. Fortunately, in many cases the hallucinations or delusions go away when the offending medication is removed or changed, such as by adjusting the dose.
Psychosis Due to a Medical Condition
There are many medical problems in which psychotic symptoms—especially hallucinations and delusions can occur. Among them are:
- Head Injuries—Traumatic brain injuries increase the risk of psychosis in the months and years following the head injury.
- Neurological Disorders—Having Alzheimer’s disease or other type of dementia, stroke, brain tumor, epilepsy, and Parkinson’s disease may increase the risk for psychotic episodes.
- Infections—Some cases of chronic infections, such as Lyme disease, syphilis, and HIV/AIDS as well as strep, mycoplasma pneumonia, herpes simplex, toxoplasma gondii, and fungal infections have been associated with psychotic episodes.
- Hormonal Changes—The hormonal changes that occur during puberty put adolescents and young adults at greater risk of developing psychosis, as does the decline in estrogen for women approaching menopause.
- Sleep Deprivation—Chronic insomnia can lead to psychotic symptoms. Research has found that symptoms can appear after 24 hours without sleep and will worsen with continued sleeplessness.
- Autoimmune Diseases—Having an autoimmune disease can increase the risk for psychosis. Researchers have found many possible contributing factors, including:
- Environmental allergens—pollen, dust mites, mold
- Exposure to toxins
- Food allergens—dairy, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans are the top 8, according to the FDA
- Lack of exercise or excessive exercise
- Leaky gut
- Obesity
- Poor diet or nutrient deficiencies
- Sleep disorders
- Stress
“With A Better Brain Comes A Better Life”
– Daniel G. Amen, M.D.
Schizophrenia & Schizoaffective Disorder: Links to Other Conditions
Emerging scientific evidence shows that schizophrenia and schizoaffective disorders are linked to other conditions and issues, including the following.
Link Between Schizophrenia and Lyme Disease
Many people with resistant psychiatric conditions, such as schizophrenia have been exposed to infectious agents that damaged their brains. In 1994, the Schizophrenia Bulletin published an image comparing the areas of the United States with the highest rates of Lyme disease and schizophrenia. They were nearly identical.

At Amen Clinics, we’ve treated hundreds of patients who came to us with resistant psychiatric symptoms, and subsequently tested positive for Lyme disease. They were helped significantly when we treated their underlying Lyme infection. A 2014 study reported that the antibiotic minocycline, used to treat Lyme disease, was found to decrease symptoms of schizophrenia in a 12-month period.
Link Between Schizophrenia and Other Infections
Other infections also have a connection to schizophrenia and other conditions. In an important study from Denmark, patients who had infections, even those that did not require hospitalization, had a higher incidence of schizophrenia and depression. Infections that have been linked to schizophrenia include:
- Strep
- Mycoplasma pneumonia
- Herpes simplex
- Toxoplasma gondii—a tiny single-celled parasite that is often carried in cats and shed in their feces
- Fungal infections
Link Between Schizophrenia and Autoimmune Disease
Many autoimmune illnesses are linked with psychiatric issues. For example, having an autoimmune disease is associated with a 45% increased risk for schizophrenia. Researchers are still trying to pinpoint the exact causes of autoimmune disorders, but many factors can play a role in their development, including:
- Leaky gut
- Environmental allergens—pollen, dust mites, mold
- Food allergens—dairy, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans are the top 8, according to the FDA
- Toxins
- Obesity
- Head trauma
- Lack of exercise or excessive exercise
- Poor diet
- Nutrient deficiencies
- Stress
- Sleep disorders
Link Between Schizophrenia and Gluten
Gluten sensitivity and celiac disease are related to a number of psychiatric disorders and symptoms, including schizophrenia. A growing body of evidence suggests that nutritional treatment may help prevent, treat, or improve schizophrenia, schizoaffective disorder, and other conditions, such as depression, bipolar disorder, anxiety, ADHD, autism, and addiction. Adopting a gluten-free diet has been associated with improvements in people with mental health conditions. Research found a decrease, or even full remission, of symptoms in a subset of patients with schizophrenia.
“When your brain works right, you work right.”
– Daniel G. Amen, M.D.
How Steve’s Schizophrenia Got Much Better
Steve’s mother brought him to Amen Clinics. Steve was homeless on the streets of San Francisco and had been diagnosed with paranoid schizophrenia and drug abuse but refused to take any medicine. He was so aggressive that he could not live at home. He was clearly psychotic when he came to our clinic and his first comment was, “I’m not going to take medicine, and you can’t make me.” He had experienced a bad reaction to medications in the past.
We told him we didn’t want him to do anything he didn’t want to do but asked if we could look at his brain, which he agreed to do. Of the more than 200,000 functional brain scans in our database at Amen Clinics, Steve’s scan was one of the worst we had ever seen, with overall low activity. (See Steve’s scan above.) When he saw it, he just stared at it for about 5 minutes, then asked, “Can you help me?”
We told him that there were better medications than the ones he had tried before and prescribed a newer antipsychotic medication and scheduled another appointment for 3 weeks later. A week later, Steve’s mother showed up in our clinic and said, “You cannot believe how much better Steve is. He is not hallucinating as much and is calmer, and we can have him live at home.”
When Steve came in for his 3-week follow-up visit, he was so apologetic for being difficult and said he felt so much better. His scan was also remarkably better. In less than one month, his brain had already improved so much.
