Lyme Disease and Other Infections
Unlike traditional psychiatry, which rarely looks at the brain, Amen Clinics uses brain imaging technology to identify patterns associated with Lyme disease and other infections.
What are Lyme Disease and Other Infections?
Lyme disease is a bacterial infection caused by the bite of an infected tick. More specifically, blacklegged ticks (also known as a deer ticks) found throughout the eastern half of the country and Western blacklegged ticks which populate the Pacific coastal areas can be carriers of Borrelia burgdorferi, the bacteria that causes Lyme disease in the U.S. It has been vastly underdiagnosed due to delayed or inadequate testing methods and a general lack of acknowledgement about Lyme disease by the medical community—especially in areas that are less vulnerable to tick-borne illnesses.
If an infection is caught early, antibiotics can often successfully treat it and diminish the chances of lasting problems. Unfortunately, many people don’t notice when they have been bitten by a tick, and not everyone who is infected with the bacteria will develop the tell-tale bullseye rash. To further complicate things, once a tick bites and is attached to the skin, it won’t cause a Lyme infection for at least 24 hours and symptoms may not emerge for a few days or even a month. Because of this delay, the possibility of Lyme disease can easily be overlooked. Furthermore, the bacteria can become dormant, hiding in cells of the central nervous system, including the brain, for months or years.
Consequently, when it remains undiagnosed, the infection festers, wreaking havoc on the immune system and causing a host of inflammatory responses which can impair healthy brain function. For example, 70% of those affected with Lyme disease report changes in their thinking, such as memory loss and reduced mental sharpness.
Who has Lyme Disease?
People who are active outdoors are more at risk for Lyme disease—especially when preventative measures to protect against tick bites aren’t utilized. Since children spend a lot of time outside, those between the age of 3 and 14 are at the greatest risk followed by people over 50, who enjoy hiking or other outdoor activities such as gardening or playing golf. Those who work outside in grassy areas or other known tick habitats are susceptible too, but anyone can get a tick bite—even in their own yard. There are an estimated 427,000 new cases of Lyme disease each year in the United States.
What are Potential Symptoms of Untreated Lyme Disease and Other Infections?
It is well known that Lyme disease and other infections can cause physiological symptoms, including fever, swollen glands, sore throat, breathing problems, headache, and joint pain or swelling. But many people are unaware that they can also lead to cognitive and neuropsychiatric issues, including:
- Poor judgment
- Memory problems
- Short attention span
- Trouble with focus & concentration
- Poor decision-making abilities
- Slower mental processing speed
- Impaired speech functions
- Changes in personality
- Hallucinations
- Problems sleeping
- Decreased libido
- Addictive behaviors
- Disorientation
- Violence
- Suicide

Lyme disease can be misdiagnosed or lead to the following if it goes untreated:
- Depression
- Bipolar disorder
- Anxiety
- PTSD
- Schizophrenia
- Psychosis
- Alzheimer’s disease
- Developmental disorders
- Autism spectrum disorders
- Eating disorders
Why Choose Amen Clinics for Treating Lyme Disease and Other Infections?
At Amen Clinics, we have extensive experience diagnosing and treating Lyme disease and other infections, and particularly the neuropsychiatric symptoms these illnesses can cause. Unlike traditional psychiatry, which remains the only medical specialty that rarely looks at the organ it treats, Amen Clinics uses brain SPECT imaging to take the guesswork out of psychiatry. Based on our brain imaging work—over 200,000 functional brain scans and growing—we can identify patterns in the brain that suggest an infection may be the root cause of symptoms.
Infected Brains Work Differently
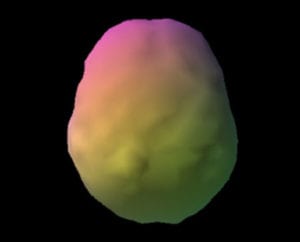
On brain SPECT scans, infections in the brain can appear as an overall pattern of significantly high or low blood flow. When these abnormal brain patterns are visible, it indicates a potentially infectious process at work. When we see evidence of infectious disease on SPECT scans, we investigate further with additional testing.
Healthy Brain Scan

Lyme Disease Brain Scan
SPECT (single photon emission computed tomography) is a nuclear medicine study that evaluates activity (blood flow) in the brain. Basically, it shows three things: healthy activity, too little activity, or too much activity. The healthy surface brain SPECT scan on the left, looking down from the top, shows full, even symmetrical activity. The scan on the right, which is of a patient with Lyme disease, shows overall decreased blood flow denoted by the bumpy appearance on the surface of the brain. The pattern on this scan shows low activity due to the infection.
Ready to learn more? Speak to a care coordinator today!
Contact UsLyme Disease & Other Infectious Agents
Lyme disease isn’t the only infection that can interfere with brain function. Other infectious agents can also cause inflammation and lead to brain disorders, which can mimic or cause a multitude of symptoms associated with mental health conditions. Because of this, people with these infections are often misdiagnosed with psychiatric disorders.
Traditionally, the medical community has dismissed the fact that infections can be associated with these types of symptoms, but that is changing. An editorial in the Journal of Alzheimer’s Disease written by a worldwide group of 33 scientists suggested the medical community has been neglecting to look at infectious diseases as a root cause of many memory problems, including Alzheimer’s disease and other dementias.
COVID-19
Many people associate the COVID-19 virus with its uncomfortable flu-like symptoms, such as sore throat, headache, fever, cough, congestion, and gastrointestinal issues. However, this virus can also have a significant and deleterious impact on brain function. Research studies have found pandemic-related increased rates of anxiety, mood, substance use, and other mental health disorders. Scientists also discovered that COVID-19 can penetrate the blood brain barrier. Likely due to an overzealous immune response that causes inflammation, the residual effects can be harmful to brain function.
While most people recover from mild or moderate cases of COVID-19 within a couple of weeks, there are many people whose symptoms persist, even after the acute infection has passed. What is known as long COVID or post-COVID syndrome can last for months. When this happens, in addition to struggling with residual symptoms such as shortness of breath, muscle pain, or inability to taste or smell things, long COVID symptoms can also include:
- Brain fog
- Fatigue
- Concentration issues
- Memory problems
- Anxiety
- Depression
- Stress
- Sleep problems
Other Infections that can Harm Brain Function
Bacteria, parasites, viruses, and other infectious agents that can cause inflammation and lead to brain disorders, include (but are not limited to):
- Streptococcus—strep throat or scarlet fever
- Toxoplasma gondii—a tiny single-celled parasite that is often carried in cats and shed in their feces
- Fungal infections—commonly an overgrowth of Candida albicans, a yeast found in the mouth, gut, and genitals
- West Nile virus—a mosquito-borne disease
- Meningitis—inflammation of the tissues surrounding the brain and spinal cord
- Herpes family viruses, such as Epstein-Barr, cytomegalovirus, herpes simplex virus-1 (most often as cold sores), and herpes simplex virus-2 (genital or buttock lesions)
- HIV/AIDS
- Syphilis
- Other tick-borne illnesses, including Rocky Mountain spotted fever, anaplasmosis, ehrlichiosis, and Powassan virus
- Helicobacter pylori (common cause of peptic ulcers)
- Chlamydophila pneumoniae (type of bacteria that causes pneumonia)
- Influenza—the common flu bug
Neuropsychiatric Symptoms of Streptococcus and Toxoplasma Gondii
Like Lyme disease and COVID-19, other infections can cause neuropsychiatric symptoms. For example,
Streptococcus bacterial infection that leads to PANDAS (pediatric autoimmune neuropsychiatric disorder) can cause a sudden onset of symptoms, such as:
- Obsessive thoughts
- Compulsive rituals
- Overwhelming fears
- Moodiness or irritability
- Motor or vocal tics
- Hyperactive behavior
- Motor skill problems
Streptococcus infection can be misdiagnosed as or lead to:
- Obsessive-compulsive disorder
- Tourette’s syndrome
Toxoplasma gondii can cause cysts to develop in the brain and other organs, leading to a condition called toxoplasmosis. Symptoms include:
- Impulsive behavior
- Dramatic mood swings
- Hallucinations
- Memory problems
- Anxiety
- Depression
- Obsessive thoughts
- Compulsive rituals
- Suicidal thoughts
Toxoplasma gondii can be misdiagnosed as or lead to:
- Schizophrenia
- Bipolar disorder
- Anxiety
- Depression
- Alzheimer’s disease
- Parkinson’s disease
- Obsessive-compulsive disorder
The Consequences of Improper Diagnosis and Treatment
When people with undetected Lyme disease or other infections are misdiagnosed with psychiatric illnesses or cognitive dysfunction, treatments often don’t work. And in some cases, they can make symptoms worse. Without a correct diagnosis and the appropriate treatment, the infection persists, causing further injury to the brain.
This can eventually lead to trouble in all areas of your life, including decreased productivity at work, poor school performance, and problems with personal and interpersonal functioning. Without getting the right treatment, Lyme disease and other infections can steal your mind and steal your life.
For people who are not responding to treatment for their symptoms, it is very important to investigate whether an underlying infection may be contributing to the issue.
“With A Better Brain Comes A Better Life”
– Daniel G. Amen, M.D.

